WASHINGTON, DC (April 16, 2020) – As the U.S. healthcare workforce struggles to care for a rise in COVID-19 cases, there are growing reports that there are not enough workers to meet the surge in demand. Some hospitals are reporting they do not have enough respiratory therapists to operate ventilators. And rising numbers of nurses and other health care workers in New York and other states have fallen ill and are quarantined, or simply unable to report to work due to family needs.
To meet the potentially explosive demand for healthcare workers, researchers at the George Washington University Milken Institute School of Public Health (Milken Institute SPH) have created a novel tool that will help states and the federal government estimate the need for health care workers under different scenarios of patient infection rates and health worker attrition. The estimates provided by the new tool will help state and federal pandemic experts plan for large spikes in illness and potential shortfalls of key ICU personnel, such as respiratory therapists, intensivists, critical care nurses and others.
“This pandemic has put extraordinary pressure on our health workforce,” said Patricia (Polly) Pittman, PhD, director of the Fitzhugh Mullan Institute for Health Workforce Equity, which is based at Milken Institute SPH. “Our interactive tool will help identify potential worker shortages during peaks in demand. Ultimately, the information gleaned from this model will pave the way toward solutions to anticipate and prevent problem by shoring up just-in-time capacity.”
Using data from the Institute for Health Metrics and Evaluation on the projected demand for services, and data from the American Hospital Association and publicly available datasets to estimate supply, Pittman and her colleagues looked at the availability of respiratory therapists and intensivists trained to work with critically ill patients. They also plan to prepare analyses of five additional professions, all needed to care for COVID-19 patients. The tool assumes surge capacity professional to patient ratios, and allows users to modify health worker attrition rates based on local information to show potential deficits in staffing.
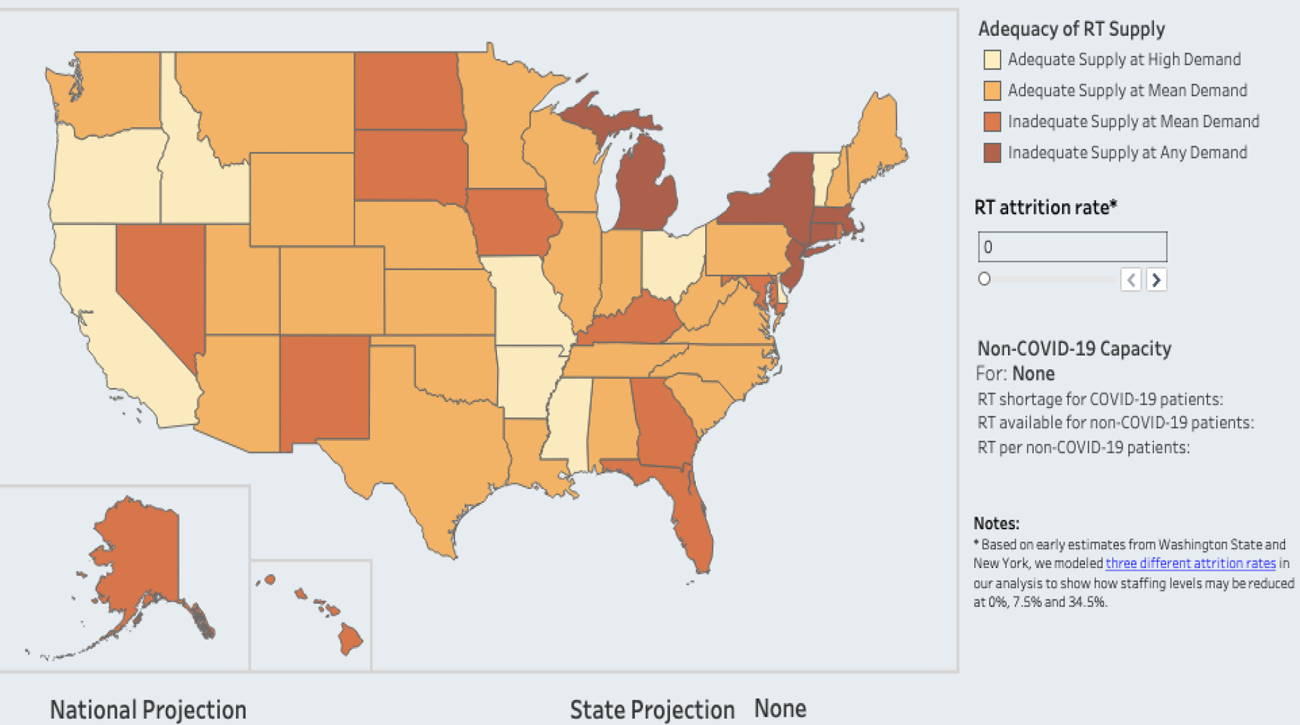
When the team plugged in estimates for respiratory therapists needed during the COVID crisis they found that five states (New York, New Jersey, Connecticut, Massachusetts, and Michigan) are at risk for not having enough of these workers even under the lowest COVID demand scenario and no workforce attrition. An additional 12 states are at risk for not having enough respiratory therapists under the mean demand scenario without any workforce attrition.
As for intensivists, three states (Louisiana, New Jersey, and New York) are at risk for not having enough even at the lowest COVID demand scenario and no workforce attrition. Ten states are at risk for not having enough intensivists under the mean demand scenario without any workforce attrition.
While other models have estimated the need for hospitalization, beds or respirators during the pandemic, this is the first tool to estimate potential health workforce deficits and surpluses, said Pittman, who is also Professor of Health Workforce Equity at Milken Institute SPH.
The tool could help state and federal policy leaders prioritize efforts to meet demands during the COVID pandemic. For example, New York and Illinois are aggressively reaching out to retired health professionals to find those willing to come back into the workforce and help out during the crisis. Other states are considering waiving training requirements or extending licensure expiration dates through the end of the pandemic.
Once the pandemic has passed, the modeling tool could be adapted to anticipate workforce needs for other emerging epidemics.
“The virus that causes COVID-19 will not be the last time we see a relatively unknown disease-causing virus start spreading in a potentially explosive manner,” Pittman said. “This tool will help public health, state and federal leaders plan for the healthcare workforce we all need to keep us all safe during this pandemic and in the future.”
To find out more about the tool and view an interactive map of shortage states click here.
The State Health Workforce Deficit Estimator is supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of an award totaling $450,000 with zero percentage financed with non-governmental sources. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by HRSA, HHS, or the U.S. Government. For more information, please visit HRSA.gov.