Study suggests people in urban areas with no exposure to livestock are becoming infected with poultry-associated MRSA via meat
Media Contact: Kathleen Fackelmann, [email protected], 202-994-8354 and Nicole Tidwell, [email protected], 614-309-1293
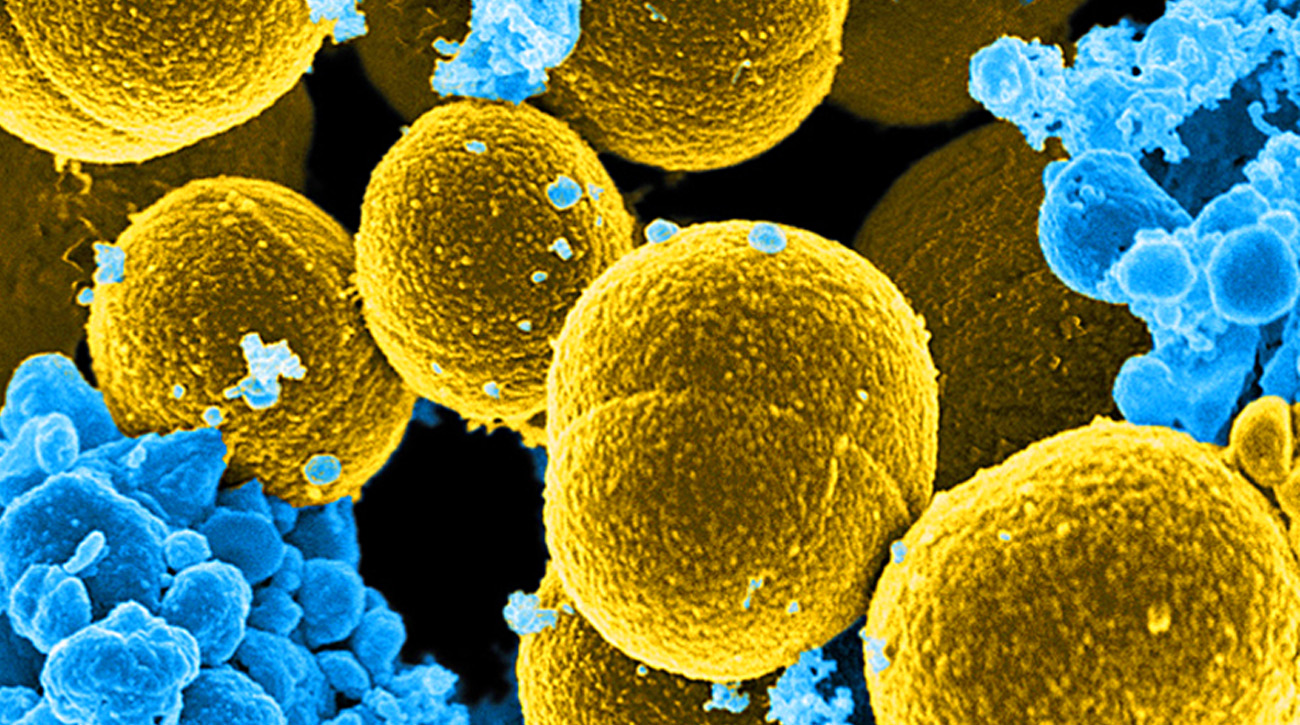
WASHINGTON, DC (September 21, 2016) — A new study offers compelling evidence that a novel form of the dangerous superbug Methicillin-Resistant Staphylococcus aureus (MRSA) can spread to humans through consumption or handling of contaminated poultry. The research, published online today in the journal Clinical Infectious Diseases, shows that poultry may be a source of human exposure to MRSA, a superbug which can cause serious infections and even death.
The study focuses on a special newly identified strain of MRSA associated with poultry. MRSA is often found in chickens, pigs and other food animals. Researchers know that farmers, farm workers, veterinarians and others working directly with livestock are at risk of MRSA infections. However, this new study, by an international team of researchers headed by Robert Skov, MD, at Statens Serum Institut and Lance Price, PhD at the Milken Institute School of Public Health (Milken Institute SPH) at the George Washington University, shows that people with no exposure to livestock are becoming colonized and infected with this new strain of poultry-associated MRSA — most likely by eating or handling contaminated poultry meat.
“We’ve known for several years that people working directly with livestock are at increased risk for MRSA infections, but this is one of the first studies providing compelling evidence that everyday consumers are also potentially at risk,” says Lance Price, PhD, Director of the Antibiotic Resistance Action Center, which is based at Milken Institute SPH, and Director of Translational Genomics Research Institute Center for Food Microbiology and Environmental Health.
“This poultry-associated MRSA may be more capable of transmitting from food to people. As MRSA continues to evolve, it may spread from animals to people in new ways,” adds Jesper Larsen, PhD, a scientist and veterinarian at the Statens Serum Institut (Denmark’s equivalent to the U.S. Centers for Disease Control and Prevention), and lead author of the paper.
The researchers reviewed the national database at Statens Serum Institut and found 10 people living in urban areas of Denmark that had been colonized or hospitalized with MRSA. Skov, Price and their colleagues then used a type of sophisticated genetic analysis to study the MRSA from those cases and compare it to strains found in people, livestock and food products from other European countries.
The researchers found:
- Ten Danes living in cities were colonized or infected with a novel strain of poultry-associated MRSA, a type of livestock-associated MRSA never identified before. None of the 10 people had worked on farms or had direct exposure to food animals.
- The strain of poultry-associated MRSA identified in the study was not found in Danish livestock but could be traced to poultry meat imported from other European Union countries.
- Isolates of the new strain found in the urban-dwelling Danes were virtually identical to each other, a finding that suggests they were all exposed from a common source — most likely contaminated poultry meat.
“Our findings implicate poultry meat as a source for these infections,” says Skov. “At present, meat products represent only a minor transmission route for MRSA to humans, but our findings nevertheless underscore the importance of reducing the use of antibiotics in food-producing animals as well as continuing surveillance of the animal-food-human interface.”
Other research suggests that modern farming practices, which often involve giving food animals low doses of antibiotics to spur their growth and compensate for overcrowding and unsanitary living conditions, has led to the rising tide of superbugs, like the new strain of MRSA identified in this study. In addition, food inspectors don’t typically test poultry and other food products for MRSA contamination and instead are focused on Salmonella and other more typical food-borne pathogens.
“We need to expand the number of pathogens that we test for in our food supply, and we need international leadership to reduce unnecessary use of antibiotics on industrial farms around the world,” Price says. “This isn't a problem unique to the EU or Denmark. Superbugs don’t respect political or geographical boundaries, so we have to work together to address this public health threat. I’m not sure that our international trade agreements are prepared to handle the specter of superbugs in meat.”
Skov adds: “I fear that if we don’t get antibiotic use in livestock under control, then new, more virulent strains of livestock-associated MRSA will emerge that pose a much greater threat to human health than what we are currently facing.”
The multi-center study, Evidence for human adaptation and Foodborne Transmission of Livestock-Associated Methicillin-Resistant Staphylococcus aureus, published today in the journal Clinical Infectious Diseases, was an international collaboration involving 25 institutions and led by researchers at the Milken Institute SPH, the Statens Serum Institute in Copenhagen, Denmark and the Translational Genomics Research Institute in Flagstaff, AZ.
Funding for this study was provided by the National Institute of Allergy and Infectious Diseases, National Institutes of Health.
About the Antibiotic Resistance Action Center: The Antibiotic Resistance Action Center (ARAC) was created to preserve the effectiveness of antibiotics by engaging in research, advocacy, and science-based policy. Learn more at our website and follow us on Twitter, Facebook and Instagram.
About Milken Institute School of Public Health at the George Washington University: Established in July 1997 as the School of Public Health and Health Services, Milken Institute School of Public Health is the only school of public health in the nation’s capital. Today, more than 1,900 students from 54 U.S. states and territories and more than 50 countries pursue undergraduate, graduate and doctoral-level degrees in public health. The school also offers an online Master of Public Health, MPH@GW, and an online Executive Master of Health Administration, MHA@GW, which allow students to pursue their degree from anywhere in the world.
About the Staten Serum Institut: Statens Serum Institut (SSI) is an institute under the Danish Ministry of Health and is the Danish National reference center for surveillance of infectious diseases and the Microbiological reference laboratory.